RABIES POST EXPOSURE TREATMENT – SIMPLE GUIDE FOR THE LAY PERSON
Rabies is a real threat in developing countries. It occurs in >100 countries and 55,000 people die from rabies each year. Risk is highest in Asia and Africa. Despite the availability of the rabies vaccination, few use them. Instead, many rely on post-exposure prophylaxis after a significant bite or scratch. Post-exposure prophylaxis is frequently expensive or unavailable at the country where the bite occurred.
I often see travelers from Indonesia who had significant exposure to rabies. Most have been exposed to dogs or monkeys. Treatment is costly, but can be life-saving. This article details WHAT TO DO AFTER EXPOSURE.
1. IMMEDIATELY CLEAN WOUND FOR 15 MINUTES
Immediately wash and flush wound thoroughly. Use SOAP, WATER, ANTISEPTICS (eg iodine or ethanol) copiously for 15 minutes.
2. ASSESS THE DEPTH OF THE WOUND
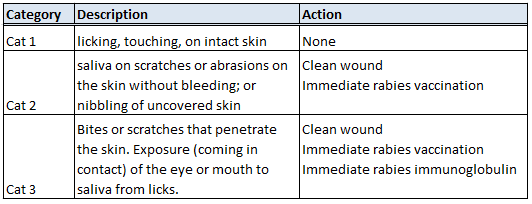
WHO classifies them into three categories based on the degree of penetration.
- Based on the category risk above act on the recommended course of action.
- If you are immunocompromised (eg organ transplant recipient, on chemotherapy, HIV / AIDS), you will require immunoglobulin in both categories 2 and 3.
- You may require antibiotic therapy especially if the wound is badly contaminated, or if you have a weakened immunity.
- Monkey bites require another post-exposure prophylaxis for Herpes B infection.
COMMON MISCONCEPTIONS
- Rabies vaccination is DIFFERENT from rabies immunoglobulin. Vaccination “trains the body” to fight the infection. This takes time (weeks). The rabies immunoglobulin provides the immediate treatment for the virus. Vaccination takes 14 days to be effective.
- Most immunoglobulins are safe. WHO recommends cell-culture derived immunoglobulins. This is a new and safe technique. The previous danger was with brain-tissue vaccine, which is being abandoned in place of the safer alternative. If you are unsure, check the label. Equine immunoglobulins have a very small risk of anaphylactic reaction (1 in 45,000). Singapore offers only humanized immunoglobulins from cell cultures.
- Pregnancy and infancy are not contraindicated. Neither is HIV / AIDS. The risk of allergy or anaphylaxis is extremely rare in humanized immunoglobulin. You would have a higher chance of winning the lottery instead.
- Waiting is not a consideration. It is an EMERGENCY. Do not wait for results.
- Follow the regimen. If in doubt, speak to your doctor.
- You still can be treated days after the bite. As a routine, we offer passive immunoglobulins up to and including the seventh day of vaccination, but not after.
To view a list of countries with Rabies, click here.
References:
- Rabies Fact Sheet. No.99 September 2011. http://www.who.int/mediacentre/factsheets/fs099/en/. Assessed 30 June 2012
- WHO position paper on Rabies. http://www.who.int/wer/2010/wer8532.pdf Assessed 30 June 2012
- Dobardzic A et al. Safety review of the purifi ed chick embryo cell rabies vaccine: data from the Vaccine Adverse Event Reporting System (VAERS), 1997–2005. Vaccine, 2007, 25:4244–4251.
- Grading table III (safety) with key references. Conclusion: moderate level of scientifi c evidence that cell-culture-based rabies vaccines are safe (http://www.who.int/entity/immunization/rabies_grad_safety.pdf).
- Wilde H et al. Purifi ed ERIG: a safe and affordable alternative to human RIG. Bulletin of the World Health Organization, 1989, 67:731–736.
- Suwansrinon K et al. Sex- and age-related differences in rabies immunoglobulin hypersensitivity. Transactions of the Royal Society of Tropical Medicine and Hygiene, 2007, 101:206–208.